Member’s story of her diagnosis through her brain injury and the symptoms she had.
Category: Health and ABI
Brain Injury and the Role of the Speech-Language Pathologist
This article discusses the role of a Speech-Language Pathologist in rehabilitation and how they can help you recover after an acquired brain injury.
No A/C? Here’s how to keep cool
Featured Image: A wooden thermometer against a blue sky. The mercury on the thermometer is 40°. The summer of 2021 … More
Cycling water bags: essential for recovery, wellness AND hydration
BY: ALISON Staying hydrated is important for maintaining one’s wellbeing. It is even more important for those who are recovering … More
How music therapy can help after brain injury
BY: KRISTA TOLOMIZENKO For many people with Acquired Brain Injury (ABI), rehab or therapy is a necessary regimen to regain basic … More
Yoga your way through the holidays
BY: ALYSON ROGERS The Holiday Season can be a challenging time for brain injury survivors for a number of reasons; … More
I chose my health over the job I loved
BY: ALYSON ROGERS For two and a half years, I worked at a social service agency for youth in Toronto. … More
Yoga Brain
BY: ALYSON ROGERS Before my brain injury, I was convinced yoga wasn’t for me; I was a year-round athlete and … More
Is the ketogenic diet the future for TBI treatment?
BY: MELINDA EVANS Ask any dietitian, and they’ll probably tell you that their clients are asking them about the ketogenic diet … More
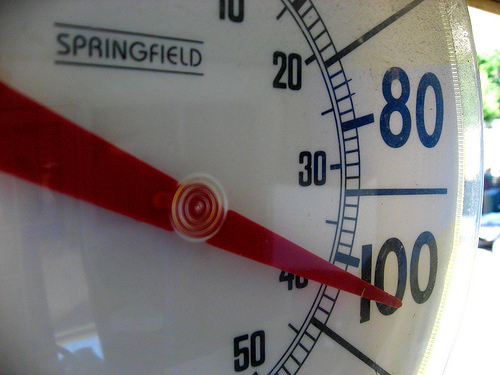
Fatigue and the heat wave
Featured Image: A close up a circular shaped thermometer reading 100 degrees. Photo credit: jo3design [DSP] May 18: Heat Wave … More










You must be logged in to post a comment.