FEATURED IMAGE DESCRIPTION: A black and white photograph of a piece of Hurricane Hazel’s damage. A dog watches intensely as … More
Category: Survivor Stories
Beauty
Discovering the beauty that surrounds us and the importance it places on us.
Survivor Stories with Lacey Fuller
This interview that was conducted with Lacey Fuller examines how she overcame her fears and struggles of her diagnosis of Post-Concussion Syndrome. She mentions how staying slightly active helped her thrive through rehabilitation and being able to return to sport.
Brain Injury Awareness from a Traumatic Brain Injury Bloomer Perspective
It messes you up this invisible injury. Making decisions and solving problems takes a lot of energy which can be challenging for people with TBI.
A Lifetime of Concussions
Jeff spent 4 years in the 1980s racing Enduro Stock Cars, which he says are the ‘lowest, cheapest, and by far the most aggressive division in short track stock car racing.’ Back then, drivers were allowed to crash into each other going 100 km/hr. Add on years of hockey and a car collision, and that’s a lot of hits to the head. Read Jeff’s story about living with Traumatic Brain Injury.
I am
I am introducing myself with two of these powerful words: “I am.” (What you choose to add after them could change your destiny for the day, for the months to come and for the rest of your life).
This day was unlike any other
BY: STELLA SLOAN This day was unlike any other. It was New Years Day; January 1, 1982 and I was … More
My name is Jaru and I am a brain injury survivor
BY: JARU My name is Jaru and I am a brain injury survivor. My name is Jaru and I am … More
Why I stopped asking ‘what if’
BY: STEVEN EDELMAN I imagine Bill Buckner must have repeatedly asked the ‘What if?’ question to himself for years after the … More
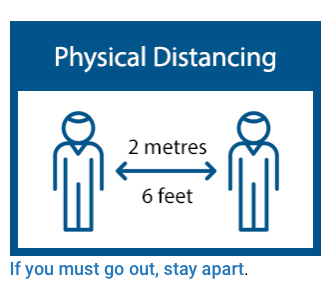
How Five Feet Apart — a story about Cystic Fibrosis – is relevant today
BY: HILARY PEARSON One thing most of us have learnt during this pandemic: germs can spread as far as six … More










You must be logged in to post a comment.